Humans of Health Care
The Canadian Health Coalition is borrowing from the powerfully engaging Humans of New York series. We bring you Humans of Health Care!
Canada’s health care system works for millions of people every day. Their stories aren’t often widely told because it’s just the system doing its job. Throughout Dr. Brian Day’s lawsuit against public health care, the Canadian Health Coalition is bringing you stories of real people helped out in times of great need by our health system.
All stories feature real people who agreed to be profiled by the Canadian Health Coalition. Names are changed if an individual wishes to remain anonymous. If you’d like to tell your story, email communications@healthcoalition.ca.
—
Erica
A cab driver was taking my husband and I to the local medical clinic in Guyana. He told us of the trouble he was in with a man who had lent him money to pay for his mother’s prescription drugs. That was just one of many clarifying moments when we realized the magnitude of the new life in Canada my husband and I were giving to two young sisters we adopted.
Thankfully, registration with Ontario’s health insurance was completed quickly and we could work on the health issues Ashena and Shania faced. I was impressed with the quick connection to the International Adoption Clinic at the Children’s Hospital of Eastern Ontario (CHEO). Comprehensive blood and immunization work was completed to bring the girls up-to-date and evaluate their health. Ottawa Public Health also followed-up with us to provide much-needed advice and guidance.
In the spring of 2014, my husband and I noticed some minor twitches in our eldest daughter, Ashena. When they didn’t subside, our nurse practitioner at our local community health centre referred us to a CHEO specialist. When the condition began to worsen, she provided a new referral with higher priority so we could be seen sooner.
With little information about the girls’ medical histories or genetics, we were at a disadvantage to pinpoint what was causing the twitches and shaking, which were by then interfering with her daily life. A specialist diagnosed her with dystonia, a rare neurological disorder that causes abnormal muscle tone and spasms. However, dystonia is a symptom of an issue and there are many different possible root causes, each with different treatment courses. Our provincial health insurance is covering comprehensive genetic testing, blood tests and MRIs to help us and the physician narrow in on where Ashena’s dystonia is coming from and how we can best help her.
Among the many things my husband Paul and I worry about, whether Canada’s public health system will be there for Ashena and Shania isn’t one of them. It’s so reassuring to know that the health care they receive is driven by what they need.
—
Ethan
(as told by his dad Joel)
I think he was 19-days-old when he had his first open heart surgery.
When Ethan was born, we thought everything was fine. We had just moved from Regina, Saskatchewan to Prince Albert. We settled in with him in our new home. One day he began to turn blue and he wasn’t breathing properly. He was in bad shape when we got him to emergency.
It’s called hypoplastic left heart syndrome. It’s a rare birth defect where the left side of the heart is really underdeveloped and can’t pump blood to the rest of the body. The lack of oxygen damaged his kidneys and liver. They told us he would have to be transported to Edmonton, Alberta to have the surgery done. He needed dialysis before he’d be strong enough for the trip. The only other option wasn’t an option at all.
At 19-days-old, Ethan had open heart surgery that saved his life — and again at seven months, and again at four years.
During one of the many hours I spent in a waiting room, I noticed a poster about health care costs in the United States — $200,000 for a heart bypass. One of the many forms I signed had costs detailed — $2,000 a day for his ICU bed, which he lived in for weeks. And here we were with no health benefits yet from a new job, living in a new province and taking our boy home with us.
We moved back to Manitoba, where we’re originally from, when he was better after the first surgery. Three different provinces have taken care of Ethan and us so well. You couldn’t guess at any of this looking at Ethan now. He’s great.
—
Craig
Over my life, I have struggled to deal with the clinical depression of bi-polar disorder. My condition ebbed and worsened over years, finally reaching a critical peak. I attempted suicide by overdosing on pills. I needed continuous dialysis for a week to repair the damage I had done to my kidneys. Such treatment is not available in Yellowknife, but through the shared services agreement with Alberta, I was transported via medevac to an Edmonton hospital.
I stayed in the city for a little longer, getting in-patient mental health support and then outpatient services. Upon my return to Yellowknife, I was provided therapy and counselling with a psychiatrist and psychologist.
There is undoubtedly stigma surrounding mental health and illness. There’s undoubtedly a lot more progress needed in our health system to properly provide care for people. But I hate thinking of a scenario where people get caught up in a cycle of mental illness and inability to pay. The worse your mental health is, the less you are able to provide for yourself, let alone pay for crucial health care services.
Public health care never gave up on me. It continued to provide me with the care necessary for my recovery. The system never stinted, it was always humane.
I’m well now. It’s nice to be well.
—
Calinda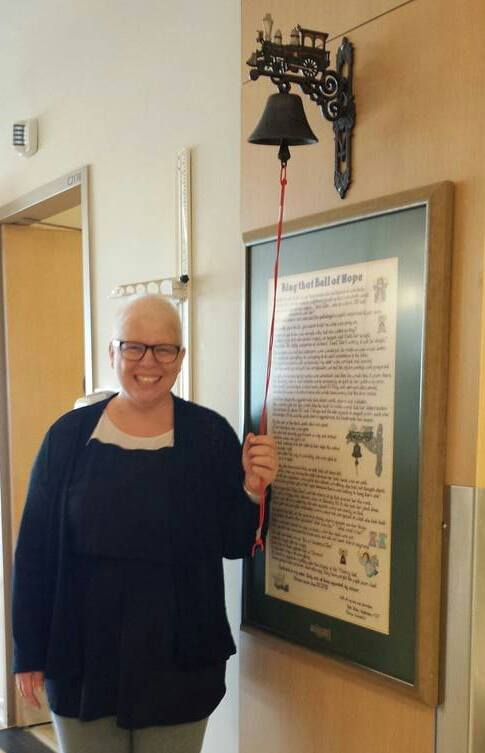
I said to myself, “That shouldn’t be there.”
My nurse practitioner confirmed that the lump I had found in my breast was something that needed to be further examined. The mammogram radiologist told me it certainly looked like cancer.
Within two weeks of the mammogram, I had a biopsy, an ultrasound, test results and a confirmation of cancer from an oncologist.
Despite the diagnosis, I didn’t want to abandon my plan to move from Ontario to Nova Scotia. I could defer starting school, but I wanted to be back on the East Coast and close to family. The team of health care providers working with me through this battle were all supportive and helped me reach my destination.
I had a tumor and pre-cancerous cells, which meant I needed a mastectomy and maybe more. Throughout all the appointments and procedures, I never once worried about my treatment plan. It wasn’t something I would have to figure out between my doctors and my insurance. I knew my health team would use every tool they had in order to do what was best for my health outcome.
The mastectomy was day surgery, and while surprising at first, it made all the difference to be able to recover in the comfort of my own home. The surgeon called my family to let them know the surgery went well. He called me the next day at home to make sure I was feeling okay. It was a relief to know follow-ups were continuing and I wasn’t alone in my recovery.
It was found that my tumor was aggressive and if a few cells had escaped, there may be new cancer developing. I was going to need chemotherapy. I finished my fourth and final round four days before moving to Nova Scotia.
Once settled in the province, the transition between care providers was easy and seamless. I was doing well and in no need of further treatment. Currently, I’m waiting for the plastic surgery that mastectomy patients are offered. It’s been expedited because of a fluid build-up issue.
All along the way, I’ve been relieved and comforted by the level of care the system and my health professionals have provided. Nothing was ever delayed waiting for insurance. I got the treatment that was right for me and right when I needed it. I always felt like there were options. I always felt the most was being done.
—
Steve*
“My story isn’t in the usual order. I got healthy, lost 60 pounds with a disciplined diet and commitment to regular exercise. Then I had a heart attack.
Walking one morning, I felt terrible and started having chest pains. Unsure what was happening, I drove myself to the hospital (I don’t recommend this). I thought I’d be in for a long wait in the emergency room, but was admitted almost immediately. Chest pains are not kept waiting. I had to stay in the hospital over the weekend waiting for a transfer to the University of Ottawa Heart Institute. I needed a coronary angiogram to determine the severity of the attack and the extent of the damage. But until then, I was on strict bedrest and monitored closely in case I had another attack.
Once at the Institute, I spent the entire day waiting only to have my surgery rescheduled because there were other new and more urgent cases. When it became obvious that I wasn’t being seen that day, I felt a little sorry for myself. Then I thought: would I rather be the guy so sick that he needed to be dealt with urgently, or the guy doing not so bad that he can wait a little longer? You see, that’s our system working the way it should. It treats people based on their needs — not on their capacity to pay.
Returning to the Heart Institute on my rescheduled date, my heart surgeon said, “You’re getting a really great stent!” They gave me an advanced one, designed to keep my coronary artery unblocked for the longest amount of time. That was a decision made by them on the basis of providing me with the best care — again, not based just on what I could pay for.”
“After surgery and a quick recovery, I was back at home. I felt like I still had a team with me, though. My family doctor, the surgeon and a case manager were all working to make sure I didn’t have another heart attack. It wasn’t enough that they fixed a problem, they were actively helping me build a long-term solution so I wouldn’t get sick again.
Aside from the actual heart surgery, the case manager helped me the most. With heart attack cases, they look at three factors: diet, exercise and stress. She saw I had already figured out the first two on my own, but that I was neglecting the third. Much like a therapist, she helped me narrow in on the pain I had in my life, emotional and mental pain that was manifesting itself physically. Without that kind of help, there’s no doubt in my mind that I would have been back in the hospital or who knows what.
Looking back at that time now, it’s amazing that everyone was just there for me. Doctors, surgeons, nurses, therapists, rehab trainers — all of them were there to help me get better. I’m self-employed and was off work for about three months. I’m lucky I could take that kind of pause from work and be okay financially. I don’t want to think about what I would have had to do if I had to pay medical bills on top of the income hit. In the US, medical expenses are the leading factor behind personal bankruptcy. A system predicated on profiting from the sick is fundamentally wrong.
Yes, every system has its inefficiencies. But ours in Canada has stood the test of time. We’re doing something right here. And as far as our economy is concerned, I see it as a secret weapon. I’m an entrepreneur who sees how Canada’s public health system helps rather than hinders people from working independently. We’re not stuck with a looming need to find secure health insurance for ourselves or our employees anywhere near to the extent as in the US. There are certainly details to work out so the system can work better for more people, but big picture, Canada’s public health system is giving us an incredible human advantage.”






GET SOCIAL: